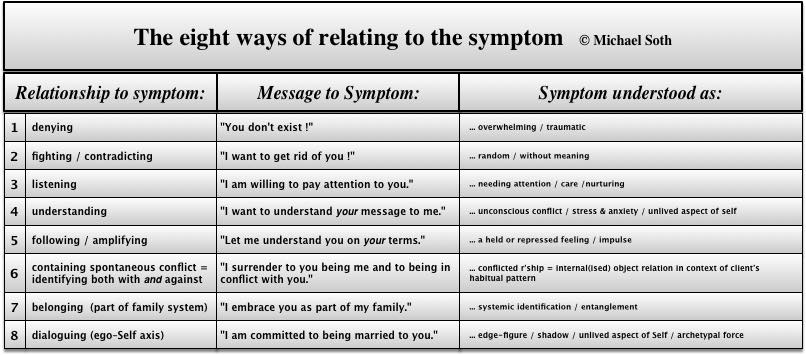
Through including body-oriented ways of working into the talking therapies, we can learn to work with many of these symptoms more directly, more deeply and more effectively (and recognise other situations where the hope of curing illness through psychology is an unreasonable idealisation). This CPD workshop is designed to expand your understanding of the bodymind connection as well as offering a wide range of creative and body-oriented techniques to include in your practice. With some illnesses - like hypertension, chest and heart problems, digestive illnesses, symptoms of the immune system - it is scientifically established that emotional stress contributes to their origin. With many other psychosomatic problems, like all kinds of pain, tinnitus, insomnia, chronic fatigue and many other unexplained symptoms, it is known that the intensity of the suffering can be ameliorated through psychological therapy that addresses the regulation and expression of emotion and de-stresses the mind. Stress is the catchall phrase that supposedly explains the influence of our psychological body-emotion-mind state on illness. However, what is less well understood, is how our bodymind does not just respond to stresses in our current situation and lifestyle, but carries accumulated stress from the past, reaching all the way back to childhood. A holistic and bio-social-psychological understanding of stress needs to include lifelong patterns of the bodymind including developmental injury and trauma (what Wilhelm Reich originally called character structures). Sometimes clients bring psychosomatic illness as a presenting issue to the therapy, sometimes these symptoms actually evolve in direct response to the unfolding therapeutic process, and the therapist gets implicated in them, e.g. “After last session I had a headache for three days!” Direct links to body sensations and symptoms as well as body image come up as part of our work in sessions every day, in so many ways: tangible pains, tensions, trembling and shaking, breathing difficulties (hyperventilation, asthma), the physical side of unbearable feelings like panic, rage, dread or terror. There are obvious somatic aspects to presenting issues such as eating disorders or addictions. And then there are the psychological implications of actual, sometimes terminal, illnesses and psychosomatic symptoms and dis-ease. How do we work with these issues and symptoms in psychotherapy? What ways are available to us for including the client’s ‘felt sense’, their embodied self states, their body awareness and sensations, their physiological experience in the interaction ? This workshop will give you a framework for thinking about the role of the body as it is relevant in your own style of therapeutic work, based upon the different ways in which clients as well as therapists relate to ‘the symptom’. Throughout the workshop, we will use roleplay of actual issues and dilemmas brought up by your clients. We will also identify and practice ways in which you can explore the emotional function and 'meaning' of your client's physical symptom or illness. Drawing on a wide range of humanistic and psychoanalytic approaches (including Body Psychotherapy, Process-oriented Psychology, various schools of psychoanalysis and Jungian perspectives) as well as the holistic paradigm underpinning most complementary therapies, we will weave together an interdisciplinary bodymind approach which is applicable within the therapeutic relationship as we know it in counselling and psychotherapy. Michael has been working with the psychological and bodymind connection of illness and psychosomatic symptoms for many years. In the 1990s he initiated a project called 'Soul in Illness', offering an integrative psychotherapeutic perspective, drawing on the wisdom which the different therapeutic approaches have accumulated regarding illness, both in terms of theoretical understanding and practical ways of working. He has run CPD workshops for therapists on ‘Working with Illness’ many times, and has developed a relational and embodied way of engaging with the client’s bodymind. In 2005 he presented for the first time his model of ‘8 ways of relating to the symptom’, which addresses the client’s own relationship to their symptom, as well as giving an overview of the different stances taken by the therapist in the various therapeutic approaches that correspond to each of the ways of relating to the symptom. These eight ways of relating to the symptom, including the corresponding theoretical understandings as well as methods and techniques for intervention, will form the underlying framework for this workshop. The bodymind connection in working with psychosomatic and physical symptoms
A weekend workshop in Athens with Michael Soth
 Even though counsellors and psychotherapists are traditionally expected to focus on emotional, mental and verbal communications, many clients invariably do bring their physical and psychosomatic symptoms into the session.
Even though counsellors and psychotherapists are traditionally expected to focus on emotional, mental and verbal communications, many clients invariably do bring their physical and psychosomatic symptoms into the session.
Calendar – One-Off CPD EventsMM2014-08-28T16:58:33+00:00
Feb
14
Sat
2026
Feb 14 @ 10:00 – Feb 15 @ 18:00
Subscribe to filtered calendar